Two recent announcements promise to put the University of Mississippi Medical Center at the forefront of Alzheimer’s disease and dementia research.
The Medical Center and four collaborating academic medical centers received $26 million in grants from the National Institutes of Health to identify risk factors for Alzheimer’s disease and related forms of cognitive decline.
UMMC also will start a new research organization: the Memory Impairment and Neurodegenerative Dementia (MIND) Center. A campaign is underway – aimed at private donations – to raise $9 million for the center’s personnel and program costs.
Initially, the center’s director plans to hire three senior scientists, three junior investigators and their staffs. In time, plans are to expand the center with cutting-edge clinical studies and patient care.
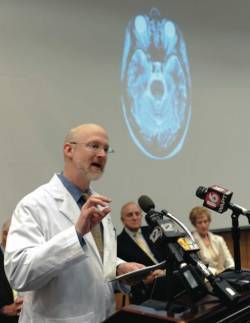
Dr. James Keeton, UMMC’s vice chancellor for health affairs, said during an announcement that the grant and center give the Medical Center the opportunity not only to address a major public health concern, but to be a leader in an increasingly important field.
“We’re here to announce two important developments that put the University of Mississippi Medical Center among the leaders in the world in research on one of the great scourges of our time – Alzheimer’s disease,” he said. “As the state’s only academic medical center, UMMC has a responsibility to meet this challenge head-on.”
The $26 million in NIH funding will pay for the ARIC Neurocognitive Study, a comprehensive examination of thousands of patients which will include detailed neurocognitive testing and brain imaging. The project, funded for four years, will build on the long-running Atherosclerosis Risk in Communities (ARIC) study, a population investigation of risks for heart disease and stroke.
Using the new exam data and the wealth of information collected during ARIC’s 20-plus years, the ARIC Neurocognitive Study is expected to further illuminate causes of dementia, giving researchers a unique window into early physiological changes that eventually culminate in Alzheimer’.
Of particular interest is the role that vascular risk factors – including hypertension, diabetes and lifestyle – experienced during middle age play in Alzheimer’s and cognitive decline later in life.
“The new ARIC Neurocognitive Study will be one of the most comprehensive investigations to date into the role of vascular and related mid-life risk factors in Alzheimer’s and cognitive decline,” said Dr. Thomas Mosley, Guyton Distinguish Professor of Medicine and the new study’s principal investigator at UMMC.
 He believes Alzheimer’s disease likely isn’t caused by a single factor, but rather by a complex process involving multiple factors interacting and accumulating over decades.
He believes Alzheimer’s disease likely isn’t caused by a single factor, but rather by a complex process involving multiple factors interacting and accumulating over decades.
“Understanding the risk factors involved in this complex process may lead to new targets for treatment,” he said. “It could also allow us to intervene at an earlier point with people who are at high risk for dementia, a time when preventative treatments may be most effective.”
Researchers at UMMC will work with four collaborating primary study sites: Johns Hopkins University, receiving about $4.6 million; Wake Forest University, receiving about $3.6 million; the University of Minnesota, receiving about $4.3 million; and the University of North Carolina at Chapel Hill, receiving about $4.6 million.
Funded under UMMC’s $9 million portion of the grant, Mosley’s team includes scientists from the Mayo Clinic, Baylor College of Medicine, the University of Texas at Houston, Boston University and Erasmus University in the Netherlands.
The original ARIC study, off which the new neurocognitive study builds, has followed a group of roughly 16,000 participants for more than 20 years, from middle age into late life. Participants were initially recruited from four communities around the U.S., including about 4,000 African-Americans from Jackson. Through medical exams over the years, ARIC participants were extensively evaluated for diseases and factors, including heart disease, hypertension and cognitive function.
Recent research has found African-Americans may have a twofold or greater risk for Alzheimer’s compared to whites. With one of the largest and most extensively evaluated African-American study subgroups, the ARIC Neurocognitive Study will help illuminate the role of ethnic differences in relative risk for dementia.
Previous work by Mosley and ARIC colleagues indicated the importance of vascular risk factors in predicting decline in cognitive functions such as memory and processing speed. Using brain imaging, Mosley and his colleagues have also shown brain changes, such as atrophy and silent strokes, are surprisingly common even in middle-age adults, and that these brain abnormalities begin to affect cognitive functions as early as middle age.
“A key question is whether brain changes we find in midlife predict dementia later in life and, if so, whether they are caused by potentially modifiable conditions, such as hypertension,” Mosley said.
“Most studies of Alzheimer’s disease have focused on what the brain looks like at the end point of the disease, but we know that the brain begins to change long before symptoms occur, perhaps as early as middle age. What’s unique about this study is that it gives us the ability to look back in time, so to speak, to determine what factors from midlife predict cognitive decline and dementia in late life.”
The ARIC Neurocognitive Study also will bring together state-of-the-art brain imaging and new genetic technology, powerful tools in the search for the causes of dementia.
“Rapidly advancing technology helps us address fundamental questions about how and why the brain ages,” Mosley said. “We’ve put together a world-class team of leading experts representing a range of disciplines, including brain imaging, genetics, epidemiology and neurology, to illuminate factors that increase risk as well as those that may protect against dementia.”
In light of the aging U.S. population and a strong association between age and dementia risk, Mosley said it’s paramount to improve clinical care and decode factors that contribute to and protect against dementia.
“They represent some of the greatest challenges facing our medical system over the next 50 years,” he said.
Due to the grant’s scope, the ARIC Neurocognitive Study is co-funded by three NIH institutes: the lead sponsor National Heart, Lung and Blood Institute; the National Institute of Neurological Disorders and Stroke; and the National Eye Institute.
The ARIC Neurocognitive Study is the foundational study of the new MIND Center, which Mosley directs.
A capital campaign at UMMC is underway to raise $9 million for the MIND Center. As the center develops, Mosley plans to recruit additional investigators to expand research in brain aging and dementia.
The fund-raising effort is supported by an advisory board chaired by former U.S. Ambassador to Portugal John N. Palmer. The board also includes honorary chairmen Robert C. Khayat, chancellor emeritus of the University of Mississippi, and former Mississippi Gov. William Winter, along with a number of other prominent Mississippians.
Palmer called the MIND Center a rare opportunity for Mississippi to build a world-class center for biomedical research.
“As I have learned more about Tom’s work, it has become increasingly clear what a tremendous resource we have here and what it means for our understanding of the brain,” Palmer said.
Keeton said the MIND Center will pool the Medical Center’s expertise in dementia and Alzheimer’s research.
“The discoveries made here will translate into better methods of caring for people who suffer from this dreaded disease,” he said. “Establishing the MIND Center will also help the University of Mississippi Medical Center continue training new generations of health-care and research professionals to take on the challenges of diseases such as Alzheimer’s.”
For more information on the MIND Center fund-raising campaign, call the UMMC Office of Development at 601-984-2300 or visit http://giveto.umc.edu.
Jack Mazurak/UMMC